PDMS Membranes: Applications, Performance and Technological Trends in the Medical Field
2026/01/30
0
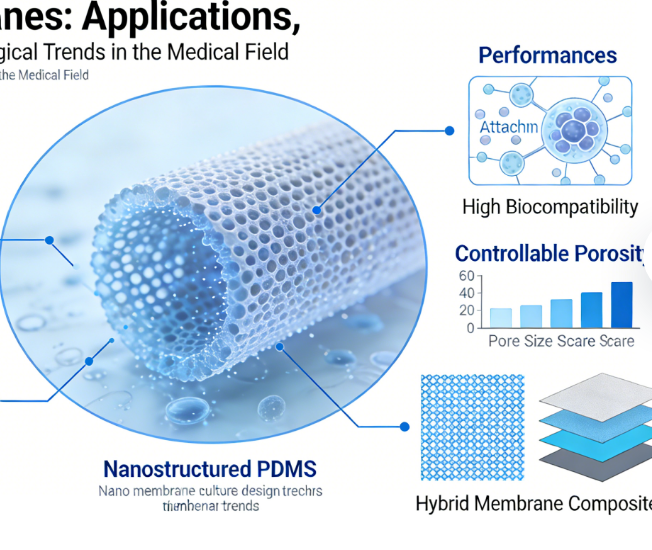
PDMS membranes have formed a diversified application system in the medical field ranging from diagnosis to treatment and from implantation to monitoring due to their excellent biocompatibility, optical transparency, tunable flexibility and easy processability, with core focus on organ-on-a-chip, microfluidics, tissue engineering, wound care, implantable devices and wearable monitoring. The following is a structured analysis of their specific applications, performance support, technical key points and development trends.
I. Core Application Scenarios and Technical Implementation
(1) Organ-on-a-Chip and Microfluidic Diagnosis
PDMS porous membranes are core components of organ-on-a-chip, used to construct bionic barriers and microenvironments for cell co-culture, supporting precise drug screening and disease modeling.
| Application Type | Technical Features | Performance and Effects | Clinical Value |
|---|---|---|---|
| Intestinal chip | 5–10μm ultra-thin porous membranes (pore size: 10–100μm or < 2μm), mechanically dynamic scaffolds, supporting intestinal epithelial-microbial co-culture | Better adaptability to mechanical stretching than PET membranes, controllable molecular permeability, and optical transparency enabling real-time imaging | Simulating intestinal barrier function, accelerating R&D of anti-inflammatory bowel disease drugs and absorption evaluation |
| Lung chip | Large surface area PDMS membranes (roll-to-roll manufacturing), gas exchange interface, integrated microfluidics | High O₂/CO₂ exchange efficiency, capable of simulating lung injury and repair | For therapeutic evaluation of acute respiratory distress syndrome (ARDS) and development of artificial lung prototypes |
| Tumor chip | Porous membranes separating tumor-stromal cells, dynamic flow fields simulating in vivo microenvironments | Increased tumor spheroid formation rate, drug responses more consistent with in vivo conditions | Screening of personalized chemotherapy regimens, reducing the cost of clinical trial and error |
| Microfluidic diagnostic chip | PDMS membranes as filtration/capture layers, suitable for single-cell analysis and nucleic acid detection | Rapid isolation of circulating tumor cells (CTCs), limit of detection reaching 10 cells/mL | Early diagnosis and prognostic monitoring of cancer |
Key Processes: Preparation of porous membranes via two-dimensional phase separation; surface modification by O₂ plasma to improve hydrophilicity and cell adhesion; sacrificial layer-assisted demolding to ensure membrane integrity and repeatability.
(2) Tissue Engineering and Regenerative Medicine
PDMS membranes serve as cell culture scaffolds and tissue regeneration templates, balancing mechanical adaptability and bioactivity regulation.
- Skin repair: Electrospun PDMS nanofiber membranes compounded with silver nanoparticles (AgNPs) and rosemary extract construct integrated wound patches with antibacterial, antioxidant and glucose-sensing functions, promoting the healing of diabetic chronic ulcers. Fluorescent probes enable real-time monitoring of glucose levels in wound beds.
- Vascular tissue engineering: PDMS microchannel membranes simulate the vascular endothelial microenvironment, and dynamic flow fields induce the alignment of endothelial cells, which is applied to the R&D of vascular grafts and improves the patency rate after implantation.
- Nerve repair: PDMS flexible membranes loaded with neurotrophic factors guide the growth of nerve axons, used for spinal cord injury repair and reducing the risk of scar tissue formation.
(3) Implantable Devices and Medical Coatings
Relying on flexibility and biocompatibility, PDMS membranes are used for surface modification and functional encapsulation of implantable devices.
- Implant coatings: PDMS membranes are coated on the surfaces of cardiac pacemakers, artificial joints and other devices, reducing foreign body reactions and fibrosis, improving the stability of long-term implantation, and providing lubricity to reduce wear.
- Drug delivery devices: PDMS membranes act as controlled-release barriers for implantable insulin pumps, regulating the release rate through membrane thickness and porosity to achieve long-acting and stable drug administration.
- Artificial cornea: PDMS membranes compounded with collagen feature optical transparency and air permeability, adapt to corneal curvature, and serve as a temporary substitute for severe corneal injury, gaining time for corneal transplantation.
(4) Wearable Medical Monitoring
PDMS membrane-based flexible sensors fit closely to the skin and realize real-time collection of physiological signals.
- Physiological parameter monitoring: PDMS membranes integrated with piezoresistive/capacitive sensors monitor heart rate, blood pressure and body temperature, which can be bent and stretched to adapt to sports scenarios, with data transmitted wirelessly to terminals.
- Sweat analysis: PDMS microfluidic membrane chips capture glucose and lactic acid in sweat with a limit of detection of 0.1mM, applicable to diabetes and sports health management.
- Wound exudate monitoring: PDMS membranes loaded with pH/oxygen sensors provide real-time early warning of infection risks, guide the frequency of dressing changes, and reduce complications of chronic wounds.
II. Performance Advantages and Technical Bottlenecks
(1) Core Advantages
- Biocompatibility: Compliant with ISO 10993 standards, with a cell viability > 90% (MTT assay) and no obvious inflammatory response after long-term implantation.
- Optical transparency: Light transmittance > 90% in the wavelength range of 400–800nm, compatible with fluorescence microscopy and confocal imaging, facilitating dynamic observation of cells.
- Tunable mechanics: Young’s modulus ranging from 0.1 to 10MPa, adjustable by the ratio of PDMS to curing agent, matching the stiffness of different tissues such as skin and blood vessels.
- Easy processability: Mature processes including soft lithography, molding and 3D printing enable mass preparation of micro-nano structures with low cost and short cycle.
(2) Main Bottlenecks and Solutions
| Bottleneck | Impact | Solution |
|---|---|---|
| Strong hydrophobicity | Poor cell adhesion and non-specific protein adsorption | O₂ plasma treatment, polyethylene glycol (PEG) grafting, collagen coating |
| Small molecule adsorption | Concentration distortion in drug screening | Surface fluorination treatment, PDMS-glass composite membranes, reducing the adsorption rate to < 5% |
| Long-term stability | Slow in vivo degradation, potentially inducing foreign body reactions | Compounding with biodegradable materials (e.g., PLGA) to prepare absorbable PDMS composite membranes that degrade 6–12 months after implantation |
III. Technical Standards and Cases
(1) Key Standards
- Biocompatibility: Compliant with ISO 10993-5 (cytotoxicity) and ISO 10993-10 (irritation).
- Membrane performance: Porous membranes with a pore size distribution CV < 10%, thickness tolerance of ±1μm, and tensile strength > 1.5MPa, meeting the requirements of organ-on-a-chip and implantation applications.
- Sterility standards: EO sterilization or γ-ray sterilization to ensure the sterility of implant-grade products.
(2) Typical Cases
- Preclinical research: PDMS intestinal chips were used to evaluate the protective effect of anti-inflammatory drugs on the intestinal barrier, with the results showing an 85% correlation with clinical trials and shortening the R&D cycle by 30%.
- Product translation: PDMS wound patches have obtained EU CE certification for the treatment of diabetic foot ulcers, increasing the healing rate by 40% and reducing the infection rate by 60%.
- Scientific research breakthrough: Roll-to-roll manufactured PDMS artificial lung prototypes achieve a gas exchange efficiency 1.5 times that of clinical artificial lungs, laying a foundation for the development of portable artificial lungs.
IV. Development Trends
- Multifunctional compounding: PDMS membranes are compounded with nanomaterials such as graphene and MXene to improve electrical conductivity and sensing performance, applicable to wearable medical devices and intelligent implants.
- Biodegradability: PDMS-polycaprolactone (PCL) copolymer membranes balance flexibility and absorbability, solving the problem of foreign body residue in long-term implantation.
- Large-scale production: Optimization of roll-to-roll (R2R) manufacturing technology enables mass production of large-size PDMS membranes, reducing the cost of organ-on-a-chip and artificial lungs and promoting clinical translation.
- AI integration: PDMS membrane sensors are integrated with machine learning algorithms to analyze physiological data in real time, realizing early disease warning and personalized treatment guidance.
Summary
The application of PDMS membranes in the medical field has moved from the laboratory to clinical translation, and their core value lies in the combined advantages of flexibility + biocompatibility + processability, providing an innovative platform for precision medicine, regenerative medicine and intelligent monitoring. In the future, it is necessary to break through bottlenecks such as hydrophobicity and small molecule adsorption, strengthen standardized and large-scale production, and further expand their application boundaries in fields such as organ transplantation and chronic disease management.